Clinical Case Report
Comprehensive Treatment Plan for Long-Term Periodontal Therapy and Dental Reconstruction: A Decade-Long Case Report 
 Author
Author  Correspondence author
Correspondence author
International Journal of Clinical Case Reports, 2024, Vol. 14, No. 1 doi: 10.5376/ijccr.2024.14.0001
Received: 16 Nov., 2023 Accepted: 21 Dec., 2023 Published: 01 Jan., 2024
He X.L., and Chen H.F., 2024, Comprehensive treatment plan for long-term periodontal therapy and dental reconstruction: A decade-long case report, International Journal of Clinical Case Reports, 14(1): 1-13 (doi: 10.5376/ijccr.2024.14.0001)
This study meticulously documents a patient's decade-long periodontal treatment and dental reconstruction journey. The patient had been suffering from periodontal disease since middle school, which led to the loss of multiple teeth and significantly impacted his quality of life. After deciding to undergo comprehensive treatment, this study formulated a comprehensive treatment plan that included periodontal disease treatment, implantation of prosthetics in the tooth loss areas, and dental crown repair. During the treatment process, this study focused on the recovery of periodontal health, the selection and fitting of implants, and the full restoration of oral function. Continuous evaluation of the patient's oral condition revealed significant improvements, including stabilization of the alveolar bone, enhancement of occlusal force, and aesthetic improvement. This case analysis highlights the importance of personalized treatment plans and the necessity of long-term follow-up for successful treatment. Despite the significant therapeutic effects achieved, this study is limited to the observation of a single case; therefore, future research should expand the sample size, compare different treatment plans, and conduct long-term follow-up studies.
In the field of dentistry, the treatment of periodontal disease and tooth loss has always been a difficult and key point in clinical work. Periodontal disease, as one of the most prevalent chronic diseases globally, has a significant impact on patients' chewing function, aesthetics, and quality of life due to the tooth loss it causes. With the advancement of medical technology, dental implant treatment has become an effective means of reconstructing missing teeth. Especially in complex cases of multiple tooth loss, dental implants not only restore the patient's function but also significantly enhance their psychological health and social interaction abilities (Chen, 2023).
The patient's case has provided us with an excellent opportunity to observe and study comprehensive treatment for periodontal disease. Since the initial visit in 2013, the patient has undergone a 10-year-long process of periodontal treatment and dental reconstruction. During this period, the medical team not only focused on the treatment of individual teeth but also placed significant emphasis on restoring overall oral function and improving the quality of life.
The choice of studying the patient's case is driven by several factors. On the one hand, his case encompasses the entire treatment process from initial periodontal therapy to the reconstruction of multiple teeth. On the other hand, his case illustrates the significance of a multidisciplinary collaborative treatment approach in addressing complex oral diseases. In clinical practice, periodontal treatment and dental implantation are typically viewed as relatively independent specialized fields. However, the patient's case tightly integrates these two areas, presenting a treatment path that spans from periodontal rehabilitation to functional reconstruction (Carvalho et al., 2021).
This study aims to explore the feasibility, effectiveness, and patient satisfaction associated with multiple-tooth implant reconstruction on the foundation of long-term periodontal treatment by reviewing and analyzing the patient's treatment history. We intend to provide a more systematic and comprehensive treatment reference for similar cases through this study, and also hope to provide new clinical insights and evidence support for the oral functional reconstruction following periodontal disease treatment.
Clearly, the patient's case is not just a record of a singular treatment process but rather a case study that involves interdisciplinary collaboration and the implementation of comprehensive treatment strategies. Through a thorough analysis of this case, we hope to provide richer treatment experiences and research data for clinical practice, and make subtle contributions to the development of oral medical work in the future.
1 Case Report
1.1 Patient basic information
The patient is a male, born in 1963, and was initially seen at the age of 51. The patient reported experiencing cavities since high school, and as he aged, dental issues gradually accumulated. By 2014, he had already lost several teeth (7 teeth), affecting his daily chewing function and quality of life.
1.2 Initial oral condition description
On August 30, 2014, during the patient's first visit to our hospital, the oral examination revealed the absence of multiple teeth, particularly in the posterior mandibular region, with noticeable tooth loss. A panoramic radiograph (OPG) examination showed, in addition to missing teeth, issues such as alveolar bone resorption, irregular tooth alignment, and periodontal inflammation.
1.3 Patient's periodontal history
Based on the patient's provided medical history and oral examination, the patient has had cavities since high school. Due to a lack of effective oral hygiene habits and regular oral care, periodontal disease gradually developed. Years of untreated periodontal disease led to the looseness and loss of multiple teeth, accompanied by a decline in alveolar bone density, further exacerbating the deterioration of oral conditions (Emampanahi et al., 2019).
1.4 Pre-treatment diagnosis and assessment
Following a comprehensive oral examination, including periodontal probing, tooth vitality testing, and panoramic radiograph analysis, we conducted a thorough diagnosis and assessment of the patient's oral condition. The results revealed not only general alveolar bone resorption and issues with tooth alignment but also signs of periapical cysts in several tooth roots, with periodontal pocket depths generally exceeding normal values. Through a comprehensive analysis, the patient's oral condition was determined to be a severe periodontal disease, necessitating a long-term and comprehensive treatment plan to gradually restore oral function (Souza et al., 2022).
Before formulating the treatment plan, we engaged in in-depth discussions regarding treatment goals, potential treatment options, and their associated risks and complications. Considering the patient's age, the extent of the condition, and the strong desire for oral function restoration, we recommended the implementation of a long-term comprehensive treatment plan. This plan includes systemic treatment for periodontal disease, necessary tooth extractions, and subsequent dental implant reconstruction.
Upon the patient's consent, we initiated a detailed treatment process aimed at gradually controlling the progression of periodontal disease, stabilizing the alveolar bone condition, and ultimately restoring the function and aesthetics of the missing teeth through implant surgery. Next, we will provide a detailed description of each step of the treatment, along with the outcomes achieved and feedback from the patient.
In the X-ray image (Figure 1), several typical oral health issues can be observed:
|
Figure 1 X-ray photo taken on August 30, 2014, showing the patient's oral and periodontal conditions |
1) Mandibular tooth loss: Left side (from the patient's perspective): 36, 37 missing teeth; Right side: 46, 47 missing teeth.
2) Maxillary tooth loss: Left side (from the patient's perspective): Elongation due to missing opposing teeth; Right side: 14 and 17 missing teeth.
3) Alveolar bone condition: In the areas where teeth are missing, the horizontal level of the alveolar bone appears to have decreased, a common consequence of long-term tooth loss. Alveolar bone recession may affect future restorations, such as dental implants.
4) Potential tooth displacement: The space created by missing teeth may lead to the displacement of remaining teeth, which could impact bite alignment and the normal function of the jaw.
2 Treatment Plan
2.1 Formulation of treatment objectives
In the comprehensive treatment plan for periodontal disease and dental implants, establishing clear treatment objectives is a crucial initial step. For the patient, the ultimate goal of treatment is to restore chewing function, enhance quality of life, and aesthetically rehabilitate the missing teeth as much as possible. In the initial phase of treatment planning, we formulated the following specific treatment objectives: firstly, to control and cure periodontal inflammation, halting the further progression of periodontal disease; secondly, to restore the function and appearance of missing teeth through dental implant surgery; thirdly, to ensure the long-term stability of the implants and the overall health of the oral cavity.
2.2 Periodontal treatment plan
In the patient's treatment plan, periodontal treatment, as a fundamental treatment step, is crucial for the success of subsequent implant treatments. The periodontal treatment plan is divided into the following steps:
Firstly, thorough removal of dental plaque and calculus is conducted to reduce the bacterial load in the oral cavity. Subsequently, deep cleaning procedures, including root planing and scaling, are performed to eliminate periodontal pockets and reduce the invasion of periodontal bacteria. Following this, necessary repair or reconstruction surgery is performed on the periodontal tissue, such as periodontal flap surgery and bone regeneration surgery, are carried out to restore the health of the periodontal tissues. Based on these interventions, patients are guided to establish good oral hygiene habits, undergo regular periodontal maintenance treatments to sustain the treatment effects (Pei et al., 2022).
2.3 Dental implant plan design
After achieving stability in periodontal treatment, the patient progresses to the phase of dental implantation. The design of the implant plan must take into account individual differences in patients, such as oral anatomical structures, alveolar bone density, and the patient's occlusal forces.
In this case, the design of the implant plan is primarily based on precise oral CT images, assessing the height, width, and density of the alveolar bone to determine the optimal position and angle for the implants. Considering the significant tooth loss in the patient, we opted for an implant system with high adaptability and stability. Additionally, personalized dental crowns were designed to maximize functionality and aesthetic effects. The implant surgery employed minimally invasive techniques to minimize surgical trauma and expedite the healing process (Wu et al., 2021).
2.4 Anticipated risk and complication management
Any dental treatment carries certain risks and potential complications, and the patient's treatment plan is no exception. In the treatment planning, we pay special attention to the management of the following aspects of risk:
1) Infection control: Strict aseptic procedures are employed, and antibiotics are administered to prevent postoperative infections.
2) Implant failure: The risk of implant failure is reduced through precise surgical planning and techniques, along with the use of high-quality implant materials.
3) Nerve damage: Risk to nerves is avoided through precise imaging localization and surgical planning.
4) Insufficient bone: In areas with insufficient bone, bone augmentation or transplantation procedures are undertaken to provide an adequate implant foundation.
5) Crown fabrication and fit issues: Digital crown design and fabrication processes are adopted to ensure crown adaptability and precise occlusion.
Through the comprehensive risk assessment and management plan outlined above, we have provided the patient with an efficient and secure treatment plan, ensuring the smooth progression of the treatment process and the ultimate success of the treatment.
3 Treatment Implementation
The treatment implementation for the patient in this case includes several phases, such as periodontal treatment, implant surgery, crown fabrication and fitting, as well as subsequent follow-up plans and oral maintenance. The following will provide a detailed overview of the execution process for each stage.
3.1 Specific steps of periodontal treatment
The patient's periodontal treatment began with a thorough oral examination and disease assessment, diagnosing them with moderate to severe periodontal disease. Treatment initially involved fundamental periodontal therapy, including the process of scaling and root planing to remove plaque and calculus beneath the gums and on the tooth roots. To control periodontal inflammation, localized antibiotic treatment was employed, and the patient was guided on appropriate oral hygiene habits (Xiang and Xiang, 2023).
After the completion of fundamental treatment, an assessment of the treatment outcomes revealed that some deep periodontal pockets did not achieve the desired results. As a result, it was decided to proceed with periodontal surgery. The surgery involved pocket reduction and alveolar bone regeneration, aiming to further reduce the depth of periodontal pockets and attempt to restore the alveolar bone lost due to inflammation. Postoperative regular check-ups and maintenance were conducted to monitor the stability of periodontal conditions and uphold oral hygiene.
When comparing the CT images from August 30, 2014, and June 21, 2015 (Figure 2), we will pay attention to several aspects to identify potential changes:
|
Figure 2 The CT scan taken on June 21, 2015 shows the oral condition after nearly 10 months of periodontal treatment |
1) Alveolar bone level and quality: After nearly 10 months of periodontal treatment, we expect to see stability or improvement in alveolar bone level and an enhancement in alveolar bone quality. If the treatment is effective, the absorption of alveolar bone should slow down, and in some cases, there might be evidence of bone regeneration.
2) Signs of inflammation: Any signs of reduced inflammation, such as clearer edges of alveolar bone and no significant widening of periodontal ligament, are signs of successful periodontal treatment.
3) Tooth alignment and gaps: There may be improvements in tooth alignment and a reduction in gaps, especially if the patient underwent orthodontic treatment concurrently.
4) Status of tooth loss: During the treatment, 35 teeth were extracted, which will be reflected in the images.
5) Soft tissue condition: The condition of soft tissues, including the health of the gums, is an area where improvement is expected in the later stages of periodontal treatment, although this may not be easily observable in CT images.
Based on the two CT images provided, the following analysis can be offered: In the 2015 image, the alveolar bone in the lower jaw appears fuller compared to the 2014 image, suggesting a potential improvement in alveolar bone quality. The areas where teeth are missing do not seem to exhibit significant new changes, indicating no further tooth loss (with one tooth extracted). There are no apparent new signs of alveolar bone resorption or inflammation in the images, which may suggest an improvement in periodontal conditions. The positions of the teeth appear relatively stable, with no obvious displacement, which is favorable for implant surgery.
3.2 Implant surgery process
After stabilizing the periodontal treatment, implant surgery planning was conducted based on a comprehensive evaluation and three-dimensional simulation using full-mouth CT scans. The implant surgery was carried out in multiple stages, starting with the placement of implants in the posterior mandibular missing areas. Implants made of titanium alloy with a moderately rough surface were selected to promote osseointegration. The surgery employed minimally invasive windowing techniques to reduce tissue damage and postoperative discomfort.
In the subsequent months, the integration of implants with the bone was assessed through clinical and radiographic evaluations. Once osseointegration reached the expected standards, the missing tooth area in the upper jaw has also been implanted with implants.
Based on the CT scan images from October 2, 2015 (Figure 3), several key points regarding the implant placement (typically referred to as fixtures) can be observed. Here are some professional assessments based on the images:
|
Figure 3 The CT scan image on October 2, 2015 shows the condition of the implant |
1) Implant positions: The images show multiple implants have been placed in the mandible. They appear evenly distributed in the areas of missing teeth, aiming to restore both function and aesthetics.
2) Implant angulation: The angles of the implants appear appropriate, indicating they should be able to support future crowns and restore a normal bite. The angle of the implants is crucial for successful implantation as they need to mimic the position of natural tooth roots.
3) Osseointegration: While osseointegration cannot be definitively assessed through this scan image, the bone structure around the implants seems to show no apparent defects or abnormalities, which is generally a positive sign.
4) Implant-bone relationship: The implants seem to be well-integrated into the alveolar bone, with no obvious excessive gaps or spaces, suggesting good initial stability.
5) Soft tissue condition: The health of soft tissues (such as the gums) is not easily assessable in the image, but there are no apparent signs of soft tissue swelling or abnormalities.
6) Impact on surrounding Teeth: The natural teeth surrounding the implants do not appear to be affected, indicating no damage to the teeth due to the implant surgery.
7) Overall occlusion: It is difficult to evaluate whether the overall occlusion relationship is affected after crown installation on this image, which requires clinical evaluation and patient functional feedback.
Based on the images, the implant surgery appears to have proceeded smoothly. However, the ultimate success will depend on the subsequent degree of osseointegration and the functionality and aesthetic outcomes after the installation of the crowns. The patient should continue with regular follow-ups to monitor the stability of the implants and the health status of the periodontium. For a more precise evaluation, clinical examinations by dental professionals and possible further assessments are necessary.
3.3 Crown fabrication and adaptation
After the implant stability was achieved, the fabrication and adaptation of the dental crowns were carried out. The design of the crowns took into consideration both aesthetic and functional requirements, utilizing all-ceramic materials to replicate the color and transparency of natural teeth. The production process of the crowns involved digital impression technology to ensure a precise fit with the implants. During the adaptation process, subtle adjustments were made to the crowns to ensure the patient's comfort and bite effectiveness (Xia, 2022).
In the CT scan images from September 11, 2016 (Figure 4; Figure 5), the following professional assessments based on visual information can be made:
|
Figure 4 The CT image from March 20, 2016 shows that most of the implants have already been fitted with dental crowns |
|
Figure 5 The CT image from September 11, 2016 shows that all implants have crowns installed, but one tooth is missing in position 16 of the upper jaw |
1) Completed implants and crown restorations: Crowns have been installed on all visible implants, indicating that the patient's oral restoration process is essentially complete.
2) Missing upper first molar (16): A tooth is missing at the position of the first molar on the right side of the upper jaw. This is due to severe alveolar bone resorption of the affected tooth, which leads to food impaction with adjacent teeth after repair, affecting the long-term stability and functional recovery of the implant.
3) Implant-crown integration and occlusal relationship: The implant crowns seem to have good occlusion with surrounding teeth, which is crucial for chewing function and long-term comfort.
4) Bone structure around implants: The bone structure around the implants appears stable on the images, showing no signs of bone absorption, which is a positive indication of implant success.
5) Shape and proportion of crowns: The installed crowns match the shape and proportion of natural teeth, contributing to aesthetic preservation and functionality.
6) Impact of missing upper first molar on occlusion: The absence of the 16th tooth may affect the distribution of occlusal forces on that side, and it is recommended that further restoration be needed in the later stage.
7) Soft tissue condition: The health of soft tissues is challenging to assess in such images, but there are no apparent signs of alveolar bone or gingival inflammation.
8) Overall oral functionality: From the images, it appears that the patient's oral restoration is nearing completion, but the impact of the missing tooth (16) on overall functionality should be considered.
Based on the comprehensive assessment above, it is recommended that the patient continue regular oral health examinations and discuss with a dental professional the optimal treatment plan for the missing tooth (16) in the upper jaw. This is essential to ensure overall oral functionality and health.
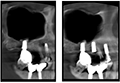
The two images depict the condition of the upper right first molar (tooth 16) before and after implantation (Figure 6). Due to limitations in image quality, the following evaluations are based on visible information in the images:
|
Figure 6 Photos of the right maxillary first molar before and after implantation on August 18, 2020 |
Before Implantation:
1) In the pre-implantation image, the absence of the tooth at position 16 is noticeable, and the alveolar bone area appears prepared for implant placement.
2) The height and width of the alveolar bone in this area seem sufficient to support an implant, but this would need confirmation through clinical measurements.
3) There is no apparent alveolar bone resorption or other abnormalities, indicating a favorable condition for implant surgery.
After Implantation:
1) The post-implantation image reveals the presence of an implant in the location of the missing tooth.
2) The implant appears to be vertically oriented in the alveolar bone, suggesting an appropriate insertion angle.
3) The density of the surrounding alveolar bone appears stable, indicating that the implant may have good bone integration.
4) No visible signs of inflammation or anomalies are present, indicating a smooth initial healing process post-surgery.
3.4 Follow-up plan and oral maintenance
After the completion of crown adaptation, a detailed follow-up plan has been established. Early follow-ups focus on monitoring the adaptation of the crown and stability of the implant. Subsequent follow-ups shift attention to long-term oral hygiene and periodontal conditions. The patient has been instructed in specialized oral hygiene maintenance, including proper tooth brushing techniques, flossing, and the use of oral irrigation devices.
Additionally, it includes regular professional cleanings and, when necessary, periodontal maintenance treatments to prevent potential recurrence of periodontal diseases and inflammation around the implants. Through these comprehensive follow-up plans and oral maintenance, the patient's oral health is well-protected, and the effect of tooth reconstruction has been maintained for a long time.
The above constitutes the complete treatment execution process for the patient, ranging from periodontal treatment to dental reconstruction. Through this carefully planned and implemented series of treatment steps, not only has the patient's oral functionality improved, but there has also been a significant enhancement in the quality of life.
4 Results Analysis
After a decade-long treatment, there has been a remarkable improvement in the patient's oral condition. The following is a detailed analysis of the treatment outcomes:
4.1 Results of combined treatment with periodontal implantation
The periodontal treatment received by the patient has yielded favorable outcomes. Through professional plaque control, periodontal surgery, and local antibacterial treatment, inflammation is controlled and the depth of periodontal pockets is significantly reduced. Following the initial periodontal treatment and maintenance, the patient's periodontal condition stabilized, laying the foundation for subsequent implant surgery. Regular follow-ups revealed significant improvements in gum bleeding and probing depth, indicating good oral hygiene and no further signs of alveolar bone resorption.
According to the CT scan images on March 20, 2023 (Figure 7), the professional clinical evaluation of the patient after completion of implant treatment is as follows:
|
Figure 7 The photo on March 20, 2023 shows a comprehensive evaluation of the patient after completing all missing tooth implants in the dental hospital |
1) Implant distribution: Implants are evenly distributed in both the upper and lower jaws, and it appears that crowns have been successfully placed on all implants, indicating full-mouth reconstruction.
2) Implant position: The position and angle of the implants seem appropriate, which is crucial for restoring tooth function and occlusion.
3) Crown appearance: The crowns installed on the implants resemble natural teeth in form, contributing to ensuring good aesthetic outcomes and functionality.
4) Alveolar bone condition: There are no apparent signs of bone resorption around the implants, implying good osseointegration.
5) Occlusion relationship: It is not possible to fully evaluate the occlusion relationship in the image, but clinical examination shows that the occlusion relationship between the crown and the opposing teeth is good.
6) Overall oral structure: The overall layout and symmetry of implants and crowns are good, essential for occlusal balance and function.
7) Restoration of missing teeth: The previously mentioned missing upper right first molar (tooth 16) seems to have been successfully restored, contributing to the restoration of bite force and function.
8) Soft tissue condition: Detailed soft tissue conditions are not easily observable in CT images, but there are no apparent abnormal signs.
In summary, the image shows a successful case of combined periodontal implantation, with good functional recovery of the implant and crown, however, the true clinical outcomes need to be determined through patient feedback, periodontal health assessments, and regular maintenance and examinations. To ensure optimal long-term results, it is recommended that Mr. Fang continues to collaborate with his dental professional for regular oral health check-ups.
4.2 Osseointegration of implants
Following the implant surgery, the osseointegration of the patient's implants is excellent. Postoperative CT scans reveal high bone density around the implants, clear margins, and no apparent bone defects. The implants exhibit a tight connection with the alveolar bone, indicating good biological compatibility between the implants and the surrounding bone structure, and a smooth osseointegration process. No signs of implant loosening or peri-implant bone resorption have been observed during the regular follow-up examinations at 3 months, 6 months, and annually thereafter (Zhao, 2023).
4.3 Functional recovery
Following implant reconstruction, the patient's chewing function has been significantly restored. Through assessments of chewing efficiency and bite force, it has been observed that the patient experiences no apparent difficulties in chewing various types of food. The restored teeth exhibit a balanced bite, without any discomfort, allowing the patient to comfortably engage in daily dietary activities.
4.4 Aesthetic effect evaluation
The fabrication of implant crowns took into consideration the patient's facial features, skin tone, and the natural color of their teeth, making the final restoration effect as consistent as possible with the height of natural teeth, beautiful and natural. The shape and color of the crowns coordinate with adjacent teeth, ensuring a natural smile line and restoring facial harmony proportions. This has significantly enhanced the patient's confidence and social comfort (Wang et al., 2023).
4.5 Patient satisfaction and improvement in quality of life
Through satisfaction surveys and assessments using quality of life questionnaires, we received positive feedback from the patient. The patient expressed high satisfaction with the treatment outcomes, particularly in terms of aesthetics and functional restoration. Additionally, the patient reported significant improvements in social interactions, daily activities, and overall psychological well-being. These positive changes further validate the success of the comprehensive treatment plan and underscore the importance of improving oral health in enhancing overall quality of life.
In conclusion, the patient's case demonstrates the effectiveness of a comprehensive treatment approach combining periodontal foundational therapy with tooth implant reconstruction. From the stability of periodontal health to the successful osseointegration of implants, and finally, to the comprehensive restoration of function and aesthetics, each step was meticulously planned and executed, ensuring the patient achieved a satisfactory treatment outcome. The success of this case provides valuable insights and reference for the treatment of similar complex oral conditions.
5 Discussion
In the realm of periodontal disease treatment and the reconstruction of missing teeth, the patient's case is a complex and typical example that spans a decade. This case not only highlights the intricacies of a comprehensive treatment approach but also underscores the critical decisions that need to be made in practical implementation.
5.1 Key decision points in the treatment process
Throughout the patient's treatment journey, the most crucial decision points included the initial comprehensive assessment and planning, the selection of appropriate timing, and the treatment approach. During the assessment, we integrated information about the patient's periodontal condition, distribution of occlusal forces, alveolar bone quality, and the patient's expectations. When planning the treatment approach, the decision was made to implement a staged treatment, starting with stabilizing the periodontal condition through foundational periodontal therapy, followed by subsequent tooth implantation.
5.2 Comparison with existing literature
According to existing literature, the success of periodontal disease treatment and tooth implantation is influenced by various factors, including individual patient differences, the selection and execution of treatment methods, and subsequent maintenance strategies (Trullenque-Eriksson et al., 2023). The patient's treatment process shares many similarities with successful cases in existing literature but also exhibits its own unique aspects. For instance, the extended duration of treatment and the complexity of the periodontal condition faced by the patient are relatively uncommon in the literature.
5.3 Key factors for treatment success
The success of this case can be attributed to several key factors: precise treatment planning and execution, high patient cooperation, and ongoing professional follow-up and guidance. Additionally, the utilization of modern dental technologies, such as three-dimensional imaging and digital treatment planning, played a crucial role in the patient's treatment.
5.4 Challenges faced and strategies implemented
Throughout the treatment process, we encountered several challenges, including insufficient height and width of the patient's alveolar bone, as well as managing the patient's psychological state during the treatment process. To address these issues, we employed bone augmentation surgery to enhance the implant foundation. Additionally, we established an interdisciplinary team comprising periodontists, oral implantologists, and a psychologist to provide comprehensive support for the patient's treatment journey.
5.5 Maintenance of long-term treatment outcomes
To sustain the treatment outcomes over the long term, we emphasize the significance of a comprehensive maintenance plan. This involves regular periodontal check-ups, professional cleanings, and education on self-oral hygiene management for the patient. Additionally, we conduct periodic assessments of occlusal forces and implant stability to prevent potential complications (Saydzai et al., 2023).
In summary, the patient's case demonstrates a successful long-term comprehensive treatment approach for periodontal therapy and missing tooth reconstruction. Through comparison and analysis with existing literature, we believe that precise planning, interdisciplinary collaboration, patient cooperation, and long-term maintenance are key to achieving treatment success. This case provides valuable clinical insights for complex periodontal cases and holds significant guiding implications for the treatment of similar cases in the future.
6 Conclusion
In this comprehensive treatment case spanning over a decade involving periodontal therapy and missing tooth reconstruction, we have not only witnessed advancements in periodontal disease treatment and implantation techniques but also experienced the profound impact of personalized treatment plans on the oral health and quality of life of the patient. From this patient's case, we can draw the following conclusions:
Firstly, long-term periodontal treatment is crucial for patients preparing for tooth implantation. During the patient's treatment, periodontal therapy not only successfully controlled periodontal inflammation but also created a healthy oral environment for subsequent implant surgery. The outcomes of this phase laid a solid foundation for the successful implantation and osseointegration of dental implants.
Secondly, this case underscores the importance of personalized treatment plans. Tailored treatment strategies designed to address the patient's oral health condition and specific needs effectively resolved complex periodontal issues, ultimately achieving comprehensive restoration of dental function. The success of this treatment approach provides valuable insights for handling similar complex cases in the future.
Thirdly, this case also illustrates the importance of interdisciplinary collaboration in managing complex oral cases. Close cooperation between periodontics, restorative dentistry, and implantology ensured the coherence of the treatment plan and optimized treatment outcomes.
Furthermore, the patient case also demonstrates the importance of long-term follow-up for maintaining treatment outcomes. Regular follow-up examinations not only monitor the health of implants and periodontal tissues but also provide opportunities for timely intervention to prevent the development of potential issues (Chen et al., 2020).
In summary, the patient's case serves as a successful example of long-term and multi-stage oral treatment. It confirms that excellent treatment outcomes can be achieved even in the most complex oral cases through comprehensive treatment plans. Future treatments should continue to employ individualized, multidisciplinary approaches, emphasizing the importance of long-term follow-up to ensure patients attain optimal treatment results and an improved quality of life.
Through the analysis of the patient's case, we have not only summarized valuable clinical treatment experiences but also provided new perspectives and insights for future clinical research and practice, particularly in the design of comprehensive treatment plans for patients with long-term periodontal disease and missing teeth.
7 Limitations and Future Research Directions
7.1 Limitations of the study
This case report meticulously documents the entire process of the patient's journey from periodontal disease treatment to the reconstruction of missing teeth. While the outcomes suggest the success of our treatment plan, it's crucial to acknowledge certain limitations in this study. Firstly, it is a single-case study, and the results may be influenced by patient-specific factors such as individual variations, lifestyle habits, and oral hygiene practices, restricting our ability to generalize conclusions to a broader population. Secondly, lacking a control group prevents a direct comparison of the effectiveness of different treatment approaches. Additionally, despite tracking the patient's treatment outcomes for a period of 10 years, this timespan may still not cover all potential delayed issues associated with dental implants. Therefore, the assessment of long-term effects might not be entirely conclusive at this point (Jordan et al., 2021).
7.2 Suggested future research
Considering the aforementioned limitations, we propose future research to include a larger sample size and incorporate a control group for comparative analysis of different treatment methods. Furthermore, it is recommended for future researchers to employ standardized treatment protocols and assessment criteria for a more accurate measurement of treatment outcomes and patient satisfaction. Attention should also be paid to long-term monitoring of the oral health status of patients, especially for regular evaluation of implant stability and changes in surrounding soft and hard tissues.
In addition to clinical studies, future research could delve into more laboratory investigations, such as materials science, to explore implant materials that are better suited for long-term use. Simultaneously, in-depth research could be conducted on the precision of implant surgeries and the customization of crown fabrication. We also recommend conducting a systematic assessment of the improvement in patients' quality of life, including aspects such as chewing ability, speech, and aesthetics, to gain a comprehensive understanding of the impact of implant treatment on patients' lives (Ravidà et al., 2021).
In the selection of treatment plans, future research should consider economic factors, assessing the accessibility of implant treatment for different income groups, and exploring cost-effective treatment options. Moreover, we encourage interdisciplinary collaborative research that integrates knowledge from periodontology, implantology, materials science, and restorative dentistry. This collaboration aims to promote innovation and development in implant dentistry techniques.
Lastly, considering the influence of psychological factors on treatment outcomes, future research should incorporate assessments and interventions for patients' psychological well-being. Studying how psychological support can assist patients in better adapting to long-term treatment processes and enhance their satisfaction and quality of life .
Through these multidimensional and multilevel studies, we hope that the future will bring about more comprehensive, efficient, and cost-effective treatment approaches for patients with periodontal disease and missing teeth.
Acknowledgments
In the process of writing this research paper, we received valuable support and assistance. We extend special thanks to the patient for their cooperation and support in our study, as well as to all colleagues at Chenghe Dental Hospital for their professional assistance in the treatment and data collection processes. Sincere appreciation is also expressed to all individuals involved in treatment, technical support, and administrative management. Additionally, we are deeply thankful to our peer experts who provided academic guidance and advice throughout the entire research period.
Carvalho R., Botelho J., Machado V., Mascarenhas P., Alcoforado G., Mendes J.J., and Chambrone L., 2021, Predictors of tooth loss during long-term periodontal maintenance: An updated systematic review, J. Clin. Periodontol., 48(8): 1019-1036.
https://doi.org/10.1111/jcpe.13488
Chen Q.Q., Wu X., Li H., and Jiang W.W., 2020, Current status and influencing factors of loss to follow-up among moderate to severe chronic periodontitis patients with long-term periodontal therapy, Zhongguo Shiyong Huli Zazhi (Chinese Journal of Practical Nursing), 36(21): 1628-1633.
Chen R., 2023, The value of periodontal maintenance therapy in maintaining long-term periodontal efficacy, Zhongguo Shiyong Yiyao (China Practical Medicine), 18(6): 63-66.
Emampanahi M., Rad S.M., Jazi M.S., Samaei N.M., Behnampour N., Mohammadi S., and Fakhari E., 2019, Association between interleukin-10 gene polymorphisms and severe chronic periodontitis, Oral Dis., 25(6): 1619-1626.
https://doi.org/10.1111/odi.13114
Jordan A.R., Stark H., Nitschke I., Micheelis W., and Schwendicke F., 2021, Epidemiological trends, predictive factors, and projection of tooth loss in Germany 1997-2030: part I. missing teeth in adults and seniors, Clin. Oral Invest., 25(1): 67-76.
https://doi.org/10.1007/s00784-020-03266-9
Pei Q.G., Wang H.C., Li L., and Wang Z.L., 2022, Triggering receptor expressed on myeloid cells‐2 stimulates osteoclast differentiation and bone loss in periodontitis, Oral Dis., 28(6): 1652-1661.
https://doi.org/10.1111/odi.14004
Ravidà A., Galli M., Saleh M.H.A., Rodriguez, M.V., Qazi M., Troiano G., Chan H.L., Wang H.L., 2021, Maintenance visit regularity has a different impact on periodontitis-related tooth loss depending on patient staging and grading, J. Clin. Periodontol., 48(8): 1008-1018.
https://doi.org/10.1111/jcpe.13489
Saydzai S., Buontempo Z., Patel P., Hasan F., Sun C.M., Akcalı A., Lin G.H., Donos N., and Nibali L., 2023, Comparison of the efficacy of periodontal prognostic systems in predicting tooth loss, J. Clin. Periodontol., 50(3): 339-347.
Souza M.Z., Nascimento G.G., González-Chica D.A., Peres K.G., and Peres M.A., 2022, Counterfactual approach on the effect of metabolic syndrome on tooth loss: A population-based study, J. Periodontol., 93(4): 591-602.
https://doi.org/10.1002/JPER.21-0175
Trullenque-Eriksson A., Tomasi C., Petzold M., Berglundh T., and Derks J., 2023, Furcation involvement and tooth loss: A registry-based retrospective cohort study, J. Clin. Periodontol., 50(3): 339-347.
https://doi.org/10.1111/jcpe.13754
Wang Y., Han H., Na S.J., and Tu J.B., 2023, Evaluation of clinical effect of 3D printing-aided autologous tooth transplantation for repairing tooth loss, Xi'an Jiaotong Daxue Xuebao (Journal of Xi'an Jiaotong University (Medical Sciences)), 44(1): 95-99.
Wu Z.N., O'Brien K.M., Lawrence K.G., Han Y.L., Weinberg C.R., Sandler D.P., and Vogtmann E., 2021, Associations of periodontal disease and tooth loss with all-cause and cause-specific mortality in the Sister Study, J. Clin. Periodontol., 48(12): 1597-1604.
https://doi.org/10.1111/jcpe.13557
Xia X.M., Jiang Z L., and Wang D., 2022, Three-dimensional reconstruction of missed teeth crown based on mirror modeling and reverse engineering, Jixie Sheji yu Zhizao (Machinery Design & Manufacture), 12: 95-98.
Xiang P., and Xiang W.J., 2023, Observation of the effect of immediate dental implant and conventional dental implant in patients with missing tooth, Zhongguo Shiyong Yiyao (China Practical Medicine), 18(8): 56-58.
Zhao Y., 2023, Clinical observation of immediate dental implantation and conventional dental implantation in patients with tooth loss, Linchuang Yanjiu (Clinical Research), 31(12): 88-91.
. PDF(1239KB)
. FPDF(win)
. FPDF(mac)
. HTML
. Online fPDF
Associated material
. Readers' comments
Other articles by authors
. Xiaoling He
. Haifeng Chen
Related articles
. Periodontal treatment
. Tooth loss
. Dentalimplants
. Comprehensive treatment plan
. Personalized treatment plan
Tools
. Email to a friend
. Post a comment
.png)
.png)
.png)
.png)